A Scientific Deep Dive
By: Dr Zaid Matti
Musculoskeletal Medicine Specialist
FacebookTwitterLinkedInEmailShare
Musculoskeletal (MSK) disorders are one of the most common causes of pain and disability worldwide. From joint osteoarthritis and chronic tendon pain to spine-related degeneration and ligament injuries, the impact on quality of life is profound. In recent years, Platelet-Rich Plasma (PRP) has emerged as a regenerative, biologically active solution that aims to heal—not just mask symptoms.

What is PRP?
PRP is derived from a patient’s own blood. It’s prepared by centrifuging a small blood sample to concentrate platelets, which are rich in growth factors and cytokines that promote tissue repair.
Depending on how it’s processed, PRP can be tailored to contain more or fewer white blood cells (leukocytes), influencing its effect on inflammation and healing. This customisability is one of PRP’s biggest advantages in musculoskeletal medicine.
How Does PRP Work?
The therapeutic power of PRP comes from the growth factors released by platelets, including:
- PDGF (Platelet-Derived Growth Factor) – promotes cell growth and angiogenesis
- TGF-β (Transforming Growth Factor Beta) – regulates inflammation and scar tissue
- VEGF (Vascular Endothelial Growth Factor) – supports new blood vessel formation
- IGF (Insulin-like Growth Factor) and FGF (Fibroblast Growth Factor) – key players in tendon and cartilage repair
When injected into a damaged or degenerated tissue, PRP can help jumpstart the natural healing process.
Key Clinical Applications of PRP
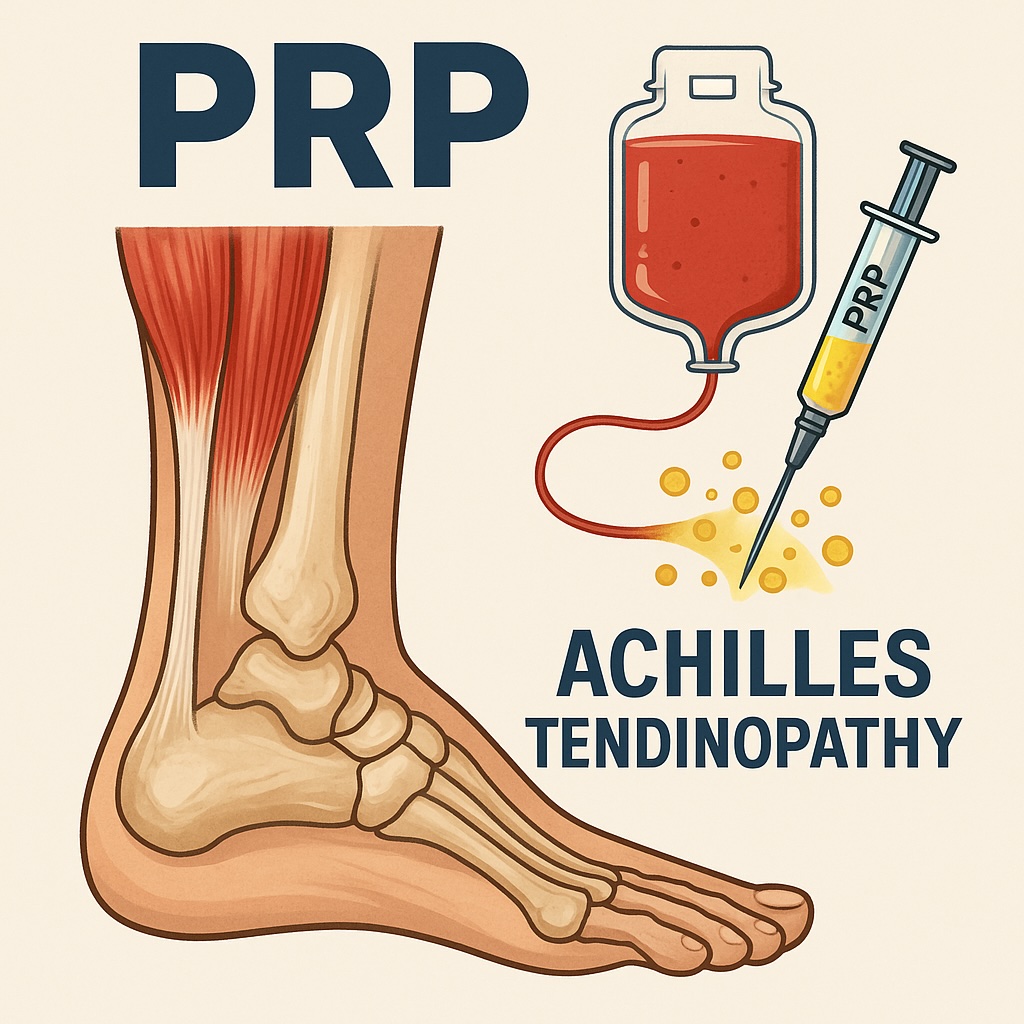
Tendinopathies
PRP has shown significant benefits in chronic tendinopathies, especially where standard treatments like physiotherapy or corticosteroids have failed.
Examples:
- Tennis elbow (lateral epicondylitis)
- Gluteal tendinopathy
- Achilles tendinopathy
- Rotator cuff injuries
Evidence: A 2021 meta-analysis in The American Journal of Sports Medicine showed PRP led to superior long-term outcomes compared to corticosteroids in tennis elbow.
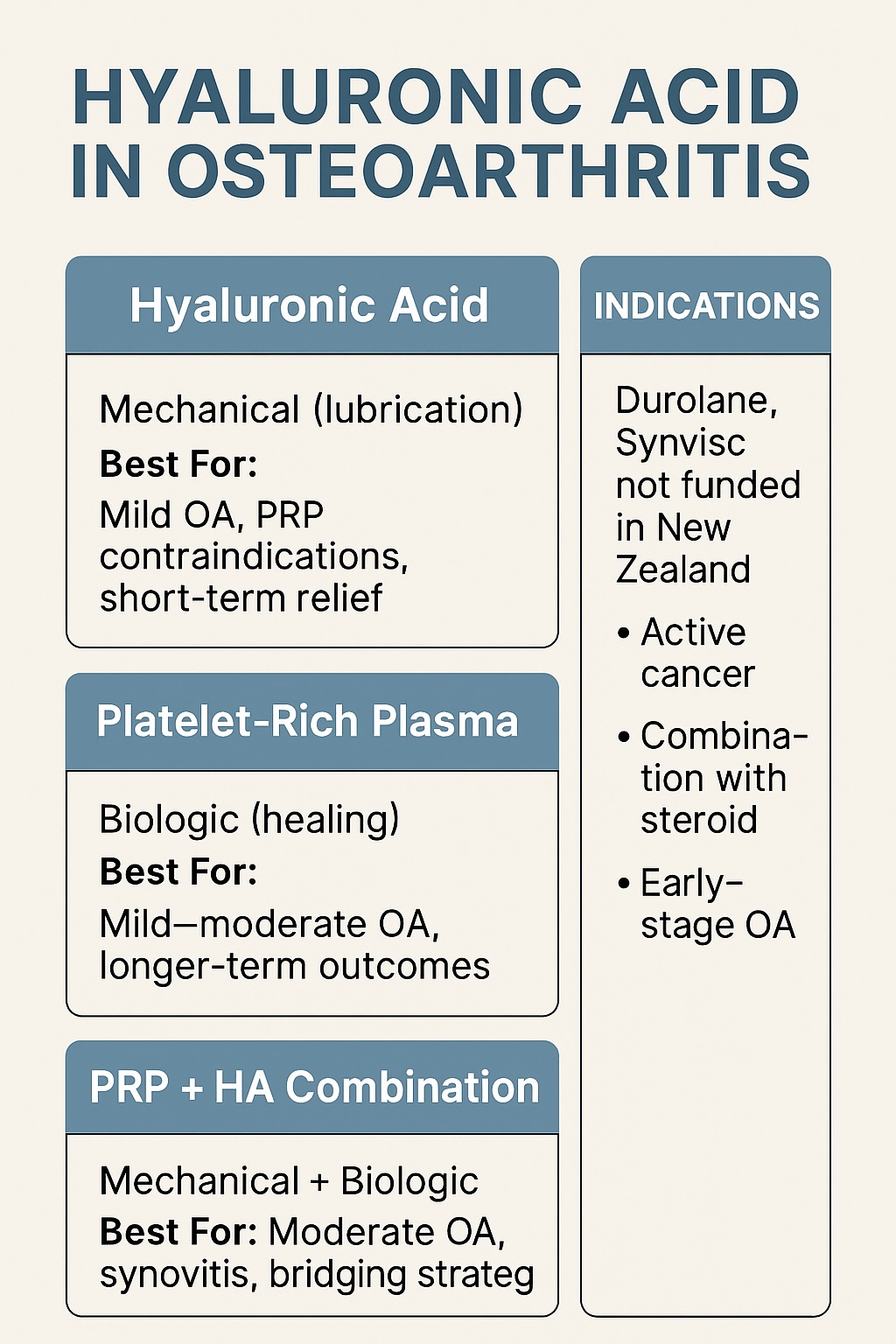
Osteoarthritis (OA)
One of the most researched applications of PRP is in treating knee osteoarthritis.
Best outcomes:
- Mild to moderate OA (Kellgren-Lawrence grade I–III)
- Early intervention before significant cartilage loss
Evidence:
- A 2019 RCT in JAMA found PRP improved knee OA symptoms significantly over saline placebo.
- A 2023 meta-analysis in PM&R found PRP was superior to hyaluronic acid and corticosteroids in improving pain and function scores.
Ligament Injuries
Used in both non-surgical and surgical settings:
Applications:
- Partial tears of ligaments (e.g., UCL in athletes)
- Augmentation during ACL reconstruction
Evidence: PRP may promote faster recovery and stronger healing in partial ligament injuries, though not a replacement for surgery in complete tears.
Muscle Injuries
Examples:
- Grade I–II strains of hamstrings, quadriceps, and adductors
Evidence: Some studies show faster return-to-play in athletes, though results vary based on timing, preparation, and injury type.
Spine-Related Conditions
PRP is gaining traction in regenerative spine medicine.
Applications:
- Lumbar discogenic back pain
- Facet joint arthritis
- Sacroiliac joint dysfunction
Evidence:
- PRP injections into lumbar facet joints reduce pain and disability better than steroids (Tuakli-Wosornu et al., 2022).
- Intradiscal PRP shows promising outcomes in early studies for discogenic pain.
Neuropathy and Nerve-Related Conditions
Emerging evidence suggests that PRP may also play a role in promoting recovery in certain neuropathic conditions. Its regenerative and anti-inflammatory properties can support nerve repair, improve vascularity, and modulate pain.
Peripheral Neuropathy
Applications:
- Entrapment neuropathies (e.g., carpal tunnel syndrome)
- Pudendal neuralgia
- Tarsal tunnel syndrome
Mechanism:
PRP may support remyelination and axonal regeneration, while reducing neuroinflammation around the injured or compressed nerve.
Evidence:
- A 2021 RCT published in Pain Medicine showed that ultrasound-guided PRP injections into the carpal tunnel were more effective than corticosteroids in improving symptom severity and functional status in patients with mild to moderate carpal tunnel syndrome.
- Other small-scale studies have reported improved sensory function and pain relief in diabetic neuropathy when PRP was injected perineurally or intraneurally.
Nerve Injuries and Post-Surgical Neuropathic Pain
Applications:
- Iatrogenic nerve injuries
- Nerve repair augmentation
- Neuromas
- Chronic post-operative neuropathic pain
Evidence:
- Animal studies and early human case series demonstrate improved nerve regeneration and reduced neuroma formation when PRP is applied at the site of nerve injury.
- A 2020 case series in Journal of Clinical Neuroscience described reduced pain scores and improved function following PRP injections for neuroma-related pain.
Is PRP Safe?
Yes. PRP is made from your own blood, which significantly reduces the risk of allergic reactions or systemic side effects.
Possible side effects:
- Mild pain or swelling after injection (a “healing flare”)
- Rare risk of infection
- No known long-term adverse effects
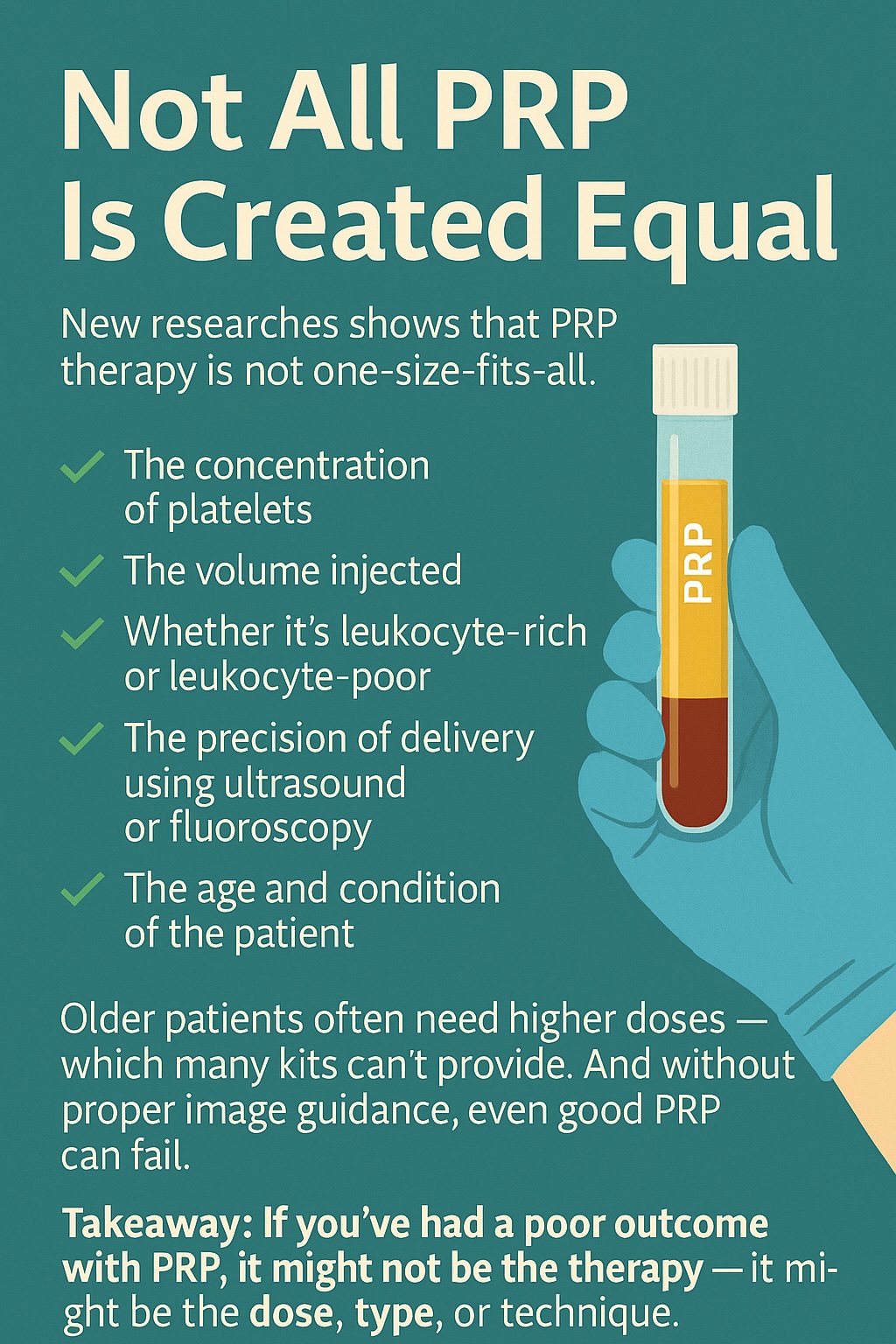
The Importance of Customisation
Not all PRP is created equal. Its effectiveness depends on:
- PRP type (leukocyte-rich vs. leukocyte-poor)
- Platelet concentration
- Use of activation agents
- Timing of treatment
- Injection technique (always use image guidance)
Tailoring these variables to each patient and condition is essential for achieving optimal outcomes.
Final Thoughts
PRP is no longer just experimental—it’s a well-supported, biologically active therapy that addresses the root of the problem in many musculoskeletal disorders. Whether you’re dealing with joint pain, tendon degeneration, or chronic spine issues, PRP may offer a safe and effective path to recovery.
We apply the latest evidence and custom PRP protocols to support your body’s own healing mechanisms. If you’re exploring regenerative options, we’re here to help.
References
- Malahias, M.-A., Johnson, E. O., Babis, G. C., Nikolaou, V. S. (2018). Platelet-rich plasma (PRP) in carpal tunnel syndrome: A systematic review and meta-analysis. Skeletal Radiology, 47(7), 953–965.https://doi.org/10.1007/s00256-018-2913-6
- Wu, Y. T., Ho, T. Y., Chou, Y. C., Ke, M. J., Li, T. Y., Huang, G. S., & Tsai, C. K. (2017). Six-month efficacy of platelet-rich plasma for carpal tunnel syndrome: A prospective randomized, single-blind controlled trial. Scientific Reports, 7, 94.https://doi.org/10.1038/s41598-017-00224-6
- Lu, L., Zhang, H., Pan, J., Song, Y., & Zhao, P. (2021). Comparison of platelet-rich plasma and corticosteroid injections in the treatment of carpal tunnel syndrome: A randomized controlled trial. Journal of International Society of Physical and Rehabilitation Medicine, 4(2), 45–52.https://journals.lww.com/jisprm/fulltext/2022/05030/a_randomized_controlled_trial_to_compare_the.2.aspx
- Moradi, A., Hasani, M., Habibzadeh, A., Aghdam, A. S. (2022). The effect of platelet-rich plasma on the outcome of carpal tunnel release surgery: A double-blind randomized clinical trial. BMC Musculoskeletal Disorders, 23, 801.https://doi.org/10.1186/s12891-022-05733-8